Covid-19 deepened the impact of Canada’s deadly opioid crisis last year, killing 17 Canadians a day on average and hospitalizing 14.
On Wednesday, the Public Health Agency of Canada (PHAC) released federal data showing a stark increase of toxic drug deaths during the pandemic, making it the deadliest year on record.
The agency warns the number of lives lost could continue to increase or remain high this year.
At the same time, there are calls for decriminalization in the hardest-hit provinces, including from a paramedic in B.C. who’s been on the frontlines during both health crises. The crisis is only getting worse, says the frontline health worker.
1,600–2,000 lives could be lost every few months
The data shows the devastating impact of Covid-19, said Canada’s top doctor Dr. Theresa Tam in a joint statement with New Brunswick’s top doctor Dr. Jennifer Russell. They’re both co-chairs on the special advisory committee on the epidemic of opioid overdoses.
“Current projections under this model suggest that we may be trending towards between 1,600 and 2,000 people in Canada losing their lives each quarter this year,” they estimated.
New #opioid-related death modelling projections show what may happen until Dec '21. Sadly, deaths may remain high or even increase.
We can help save lives and support people who use drugs through health interventions.https://t.co/JkTtve6JxO pic.twitter.com/evD689s2Tx
— Canada's CPHO (@CPHO_Canada) June 23, 2021
Last year, 6,214 people died as a result of toxic opioids compared to less than 4,000 deaths in 2019. Ninety-six per cent of toxic opioid deaths in 2020 were accidental.
According to PHAC, heightened feelings of isolation, stress, anxiety and depression combined with a toxic and unpredictable drug supply, as well as a lack of social services for people who use drugs, during the pandemic likely worsened the crisis.
Four scenarios are laid out for the remainder of 2021 based on different levels of health intervention and amounts of fentanyl in drug supplies.
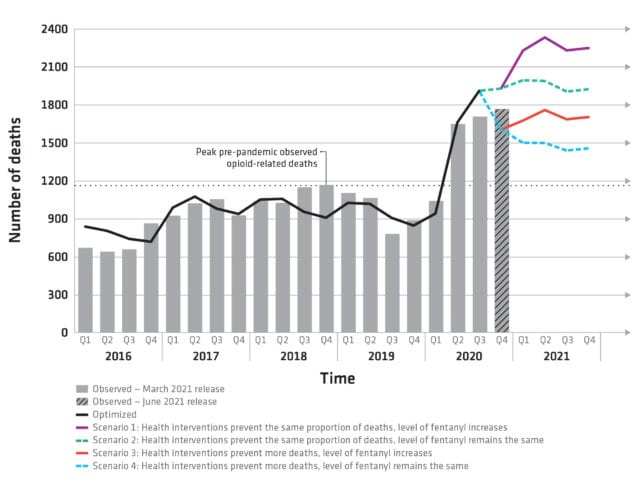
Public Health Agency of Canada outlines four possible with different levels of intervention and fentanyl in drug supplies. Chart via PHAC
National data from the last three months of 2020 suggest Canada is somewhere between Scenario 2 and 3. The former is if health intervention prevents the same proportions of deaths while fentanyl levels stay the same, and the latter is if health interventions prevent more deaths but there’s an increasing level of fentanyl.
Fentanyl was found in 82 per cent of toxic opioid deaths last year.
Pandemic isolation ‘aggravating’ overdose crisis, paramedic says
While opioid toxicity deaths have spiked across Canada, the West Coast has seen the biggest impact by far.
Eighty-five per cent of all opioid toxicity deaths between January and December of last year happened in B.C., Alberta or Ontario. The majority of deaths were among people between the ages of 20 and 49, and men accounted for 77 per cent of accidental stimulant toxicity deaths.
A paramedic with more than two decades of experience who’s working around the Lower Mainland in B.C. has felt the impact of the pandemic mixed with the toxic drug supply.
“For the last 12 to 18 months, these drugs are just stronger and stronger,” Daniel tells Mugglehead by phone. His identity is being protected so he doesn’t face repercussions at work.
On some days, there can be around seven overdoses in a matter of 12 hours on Vancouver’s Downtown Eastside, he says, noting that many people without fixed addresses come to Vancouver for the weather.
But the issue isn’t isolated to that neighbourhood.
“This problem is something that is not just hitting the vulnerable population of the Downtown Eastside — it’s happening everywhere,” he says. “One of the factors that is contributing to this is basically the isolation aggravated by the pandemic and the social distancing measures.”
The pressure on the government to change course is immense in terms of decriminalization, says Donald MacPherson, executive director of the Canadian Drug Policy Coalition.
“At this particular moment, our drug policy is so past its due date. It’s not working. Governments, the federal government in particular, really needs to chart a path forward. We need to stop pretending that tweaking drug prohibition as it is today is going to have a better outcome in the future. It won’t. It’s really a pivotal point in the history of drug policy in Canada. We’ve never seen such a catastrophic failure of the policies,” he says.
He argues the response to all drugs should be similar to legalizing cannabis in Canada and focus on safety and regulation to give adults reasonable access.
“If Covid has taught us anything, it’s that past measures don’t work. You have to do things seriously and to get rid of the toxic drug supply — there’s no signs it’s going to go away.”
Daniel also believes the only solution to ensure a safe supply is decriminalization, which would also address criminality associated with illegal trade, like gun violence.
Education around drugs is necessary, he says.
“But not education from the point of just stigmatizing drug use [but] giving meaningful scientific information to teenagers,” he argues. “It’s easier to try to educate people when you give them information, scientific or evidence-based, rather than say, ‘No, drugs are bad. Stay away from drugs.'”
2020 was the most devastating year on record for toxic drug deaths in B.C.
A total of 1,724 people were killed, a 74-per-cent increase from the year before. The province’s death toll accounted for 28 per cent of deaths in the country, despite being home to only 13 per cent of Canada’s population.
In the first four months of 2021, 680 people have already died in B.C. from toxic drugs.
Read more: BC to request federal exemption to decriminalize drug possession
Read more: BC health officials lukewarm on cannabis as harm reduction

Canada’s top doctor calls for better access to ‘life-saving services’ like safe supply programs, treatment services and take-home Naloxone. Photo by James Heilman via Wikimedia Commons.
The City of Vancouver is in talks with Health Canada about a request for a federal exemption to allow simple possession of small amounts of drugs in response to the ongoing health crisis.
Mayors in Ontario have similarly called for decriminalization. This comes after 2,426 opioid-related deaths were reported in the province in 2020. That’s an increase of 60 percent from the year before.
Chief Public Health Officer Tam calls for better access to “life-saving services” like safe supply programs, treatment services and take-home Naloxone.
“In order to urgently address the increasing substance-related harms in Canada, we must continue to recognize substance use as a health and social issue and treat people who use drugs with dignity, compassion and respect. Importantly, this means we must all work to remove barriers so that people who use drugs have access to supports they want and need,” she said in a statement.
“These actions can help save lives, and are needed now more than ever due to the compounding public health impacts of the pandemic.”
Update (2021-6-29, 10:30 a.m.): This article has been updated to include comments from the Canadian Drug Policy Coalition.
Follow Kathryn Tindale on Twitter
kathryn@mugglehead.com














