Texas-based Cizzle Bio, Inc submitted a grant application to the National Institutes of Health (NIH) in support of a two-year study validating its CIZ1B biomarker to detect early-stage lung cancer.
The company announced this application on Monday, in conjunction with its two research institutions, these being the Florida Institute for Human and Machine Cognition (IHMC) and the Southwest Research Institute (SwRI).
IHMC will develop deep learning models that link biomarker expression to cancer onset. The team will leverage its advanced computational biology infrastructure and access the University of Florida’s HiPerGator supercomputer. This collaboration will accelerate model training and improve predictive accuracy.
The NIH proposal marks a major step in Cizzle Bio’s mission to detect lung cancer before symptoms appear. Lung cancer remains the leading cause of cancer-related deaths in the U.S. and worldwide. This is largely because doctors often diagnose it at late stages.
If approved, the study will analyze pre-diagnostic and longitudinal blood plasma samples from the PLCO Cancer Screening Trial. The National Cancer Institute manages this landmark biorepository. It contains tens of thousands of blood samples from high-risk individuals, collected years before any cancer diagnosis.
Researchers will use these samples to assess whether the CIZ1B biomarker can detect lung cancer early. Additionally, they will examine CIZ1B expression to evaluate its accuracy in predicting disease onset.
Further, the study offers a rare chance to validate CIZ1B using real-world pre-symptomatic data. As a result, Cizzle Bio could transform early lung cancer detection and improve survival rates.
Read more: Breath Diagnostics gives the public the chance to join the fight against cancer
Read more: Breath Diagnostics onboards new president and closes critical financing
Study could refine screening strategies
The proposed study will analyze 1,730 lung cancer cases to evaluate CIZ1B’s performance across key subgroups. These include age, gender, ethnicity, smoking history, and other demographic or behavioral factors.
Researchers will examine whether early biomarker changes link to more aggressive disease forms. They will also assess detection accuracy across various lung cancer histological subtypes.
Further, the team aims to identify the optimal window for early detection. A key goal is to determine how far in advance CIZ1B can signal cancer before clinical diagnosis.
As a result, the study could refine screening strategies and improve outcomes for high-risk patients.
“CIZ1B has demonstrated high sensitivity and specificity in earlier studies of Stage 1 lung cancer, which were conducted by Cizzle Biotechnology at the University of York in the UK,” said William Dalton, Ph.D., M.D., senior consultant for clinical trials at Cizzle Bio.
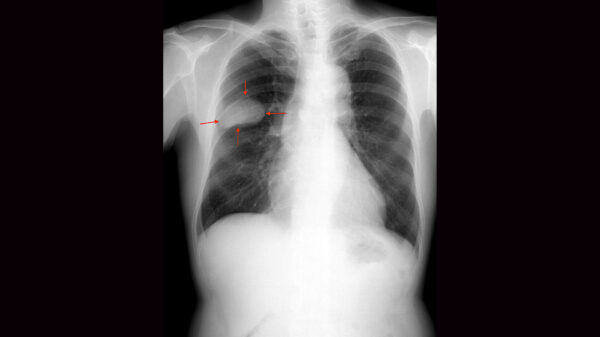
Low-dose CT (LDCT) remains the recommended method for lung cancer screening, but it carries a high false-positive rate. In contrast, the CIZ1B test uses a minimally invasive, high-throughput ELISA assay. It is well-suited for routine clinical use and scalable across healthcare settings.
The study builds on strong preliminary evidence and aims to confirm CIZ1B’s role in early lung cancer detection. In addition, it may enable earlier intervention and improved patient outcomes.
Furthermore, widespread adoption of the CIZ1B test could reduce the high costs of treating late-stage lung cancer. This represents a significant benefit for Medicare and other major payers.
Meanwhile, Cizzle Bio continues expanding its network of clinical, research, and health system partners. The company expects a response from the NIH later this year.
Read more: Breath Diagnostics pioneers novel lung cancer breath test
Read more: Breath Diagnostics takes aim at lung cancer with One Breath
There are multiple alternatives to low-dose CT
Low-dose CT remains the primary screening tool for lung cancer, but it carries risks due to radiation exposure. While effective at detecting tumors, LDCT also has a high false-positive rate, often leading to unnecessary follow-ups. As a result, researchers continue to explore safer, more accurate alternatives.
One promising approach is Breath Diagnostics’ OneBreath technology. This non-invasive test analyzes volatile organic compounds (VOCs) in exhaled breath. These compounds can reflect early biochemical changes linked to lung cancer. In contrast to LDCT, OneBreath poses no radiation risk and offers the potential for low-cost, routine screening in clinics or even primary care settings.
In addition, liquid biopsy tests are gaining momentum. These tests detect cancer-related genetic material—such as circulating tumor DNA—in the bloodstream. While still under development, liquid biopsies could identify lung cancer at earlier stages and provide insights into tumor mutations for personalized treatment.
Furthermore, autoantibody blood tests represent another potential option. These tests identify immune system responses triggered by tumor growth. Studies suggest that autoantibody panels may detect cancer years before clinical symptoms appear. They are also minimally invasive and easy to integrate into annual health checks.
While none of these methods have fully replaced LDCT, each offers unique advantages. Together, they highlight the push toward safer, earlier, and more accessible lung cancer screening. As validation studies progress, a multi-modal approach may emerge as the most effective strategy for saving lives and reducing healthcare costs.
.
joseph@mugglehead.com