Advanced imaging technology at the WVU Heart and Vascular Institute (HVI) is improving the efficacy of lung cancer bioposies for WVU Cancer Institute patients.
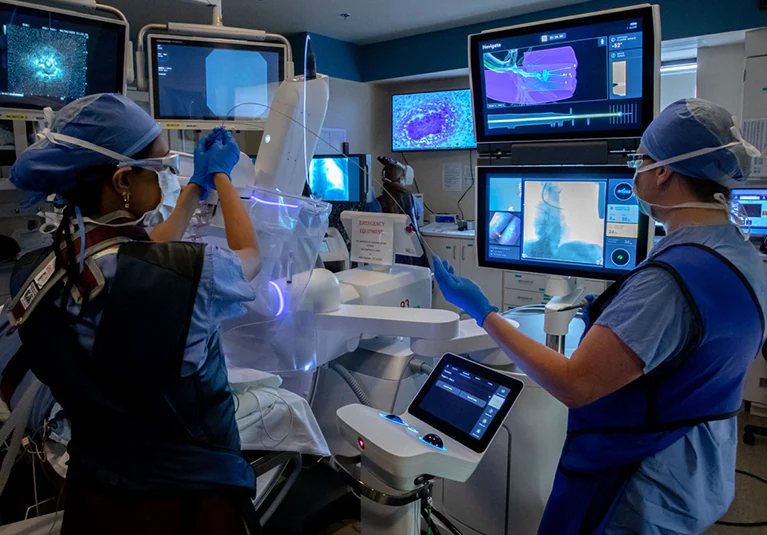
The institute is looking to implement a marriage between robotic bronchoscopy and advanced imaging technology to help usher in an era of safe, accurate and timely diagnosis and treatment, said Doctor Saiesh Voppuru, a thoracic surgeon in the HVI’s Department of Thoracic and Esophageal Surgery on Tuesday.
According to the American Cancer Society, lung cancer ranks as the leading cause of cancer deaths across the world. More people die of cancer every year from lung cancer than from colon, breast and prostate cancer combined.
Delayed diagnosis often results from low participation in screening programs and limited access to accurate, safe biopsy techniques. Because of the lung’s structure and function, biopsies can be challenging. However, advanced imaging technology at the WVU Heart and Vascular Institute (HVI) is improving accuracy for patients at the WVU Cancer Institute.
“Lung nodules appear to shift, depending on the volume of air inside the lung. We call that a CT-to-body divergence,” Dr. Voppuru said.
“CT-to-body divergence makes it harder for us to navigate to the nodule’s exact location. The doctor is basically looking at a moving target, and the bronchoscope’s catheter can miss the nodule based on its movement.”
Lung cancer often begins as a small nodule, commonly called a “spot on the lung” by patients. Other causes, such as scarring or past infections, can also produce nodules. However, many lung nodules turn out to be cancerous. Early diagnosis leads to better outcomes, as with any cancer. Time is critical. The sooner treatment begins, the better the results. Additionally, prompt intervention can reduce complications and improve survival rates.
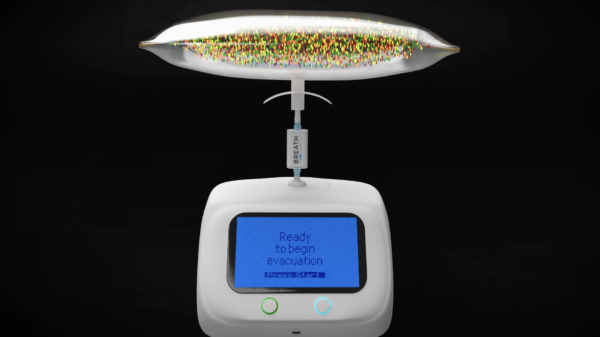
Read more: Breath Diagnostics pioneers novel lung cancer breath test
Read more: Breath Diagnostics takes aim at lung cancer with One Breath
Robotic bronchoscopy reduces risk of complications
Because lung nodules often form in the organs’ outer (peripheral) regions, their size and shape complicate access. Doctors find it harder to reach these nodules using a bronchoscope, a long, thin tube inserted through the windpipe. In such cases, they often diagnose cancerous nodules through a needle biopsy. CT imaging guides the needle through the chest wall to the nodule. This traditional method remains effective but carries risks. Additionally, it can lead to complications such as lung collapse.
Robotic bronchoscopy helps doctors reach peripheral nodules while reducing the risk of complications. However, challenges still remain. A successful lung biopsy demands high precision and control. Cone beam CT provides advanced imaging for this purpose. It offers refined, real-time visualization of lung nodules. Additionally, it improves targeting accuracy and enhances patient safety.
“Deep lung biopsies can now be performed without long needles passing through the chest wall and peripheral nodules that would otherwise be inaccessible with a traditional bronchoscopy can be targeted, thanks to the pairing of cone beam CT with robotic bronchoscopy,” Voppuru said.
Cone beam CT works much like a standard CT scan but uses a lower dose of radiation and operates directly in the OR.
The machine rotates around the patient while they lie on the table, providing real-time imaging. This allows the care team to guide the robotic bronchoscope precisely to the nodule and correct for any divergence, improving accuracy.
Traditional methods often struggle to locate the exact position of a lung nodule. As a result, some biopsies fail to deliver a clear diagnosis. Additionally, this can force patients to repeat the procedure, delaying treatment by weeks while the nodule potentially grows.
Read more: Breath Diagnostics onboards new president and closes critical financing
Read more: Wearable tech provides incomplete data for heart health
Low-dose CT can produce false positives
While low-dose CT scans offer significant benefits in detecting lung nodules and cancers early, they are not entirely risk-free. Even at reduced levels, radiation exposure can accumulate over time, especially in patients who undergo repeated imaging. This cumulative exposure may slightly increase the long-term risk of developing radiation-induced cancers. This is particularly acute in vulnerable populations such as children, young adults, or those with genetic predispositions to cancer.
Additionally, low-dose CT scans can produce false positives—nodules that appear suspicious but are ultimately benign. These findings can lead to unnecessary anxiety, follow-up tests, and sometimes invasive procedures like biopsies that carry their own risks. The psychological and physical burden of this testing demonstrates the importance of using imaging judiciously and exploring safer, equally effective alternatives.
As imaging technology evolves, the medical community continues to explore methods that minimize or eliminate radiation exposure altogether.
Techniques such as MRI, advanced ultrasound, and novel functional imaging tools offer potential pathways forward.
Furthermore, innovations like robotic bronchoscopy paired with real-time imaging technologies (e.g., cone beam CT) allow for more targeted and efficient diagnostics, reducing the need for repeated scans. The goal is to maintain diagnostic accuracy while minimizing harm, making the search for safer imaging alternatives a public health priority.
Beyond imaging, there are a handful of startups looking to produce technologies blending artificial intelligence and machine learning to produce danger-free outcomes.
Startups like Breath Diagnostics are developing noninvasive technologies to detect lung cancer through breath analysis, using biomarkers linked to cancer metabolism. Another company, Owlstone Medical, uses similar volatile organic compound detection to identify disease earlier and more accurately, aiming to replace or supplement imaging-based methods with safer, quicker diagnostics.
.